After recently writing about the use of tourniquets in crush injury scenarios, I felt it was important to return to the fundamentals: the primary use of the tourniquet as a tool for controlling life-threatening bleeding. More importantly, it seems essential to introduce—or clarify—the concept of conversion: transitioning from a tourniquet to another method of bleeding control. This step, often overlooked, is especially critical in remote settings, where evacuation delays are common and the risks associated with prolonged circulation loss increase rapidly. What follows is a structured overview of what needs to be known, assessed, and taught in the field.
Historical Perspective
Over the past two decades, the use of the tourniquet has evolved significantly. Once reserved for professionals such as military personnel or tactical teams, it is now taught more broadly, including in public first aid training. Programs like “Stop the Bleed” have raised awareness about its importance. As a result, tourniquets are now found in many more first aid kits—which is a good thing. However, this increased accessibility also brings the risk of overuse or automatic application without proper judgment.
When Should a Tourniquet Really Be Applied?
To apply a tourniquet properly, clear criteria must be followed—standards that have been validated by experts such as the Tactical Combat Casualty Care (TCCC), the Wilderness Medical Society (WMS), and reinforced in field-based training programs like those offered by SIRIUSMEDx. A tourniquet is not a routine intervention; its use must meet specific conditions, as it carries serious consequences.
A tourniquet is recommended only in situations where bleeding poses an immediate threat to life—that is, when there is a real risk of death from hemorrhage if no decisive intervention is taken. Experts recognize the following criteria:
- Active, pulsatile bleeding that does not stop despite effective direct pressure
- A traumatic amputation or major limb injury with uncontrolled hemorrhage
- An estimated blood loss of over one litre, visible on the ground or clothing
- A patient showing signs of hemorrhagic shock (pallor, sweating, agitation, rapid pulse)
- Failure of effective wound packing or a properly applied pressure dressing
This isn’t about bleeding that merely looks dramatic—there must be clear signs that circulation is compromised to the point where life is at risk. In such cases, there’s no waiting. The tourniquet is applied immediately to preserve life, and conversion is considered as soon as conditions allow.
How to Apply a Tourniquet Effectively and Safely
Applying and removing a tourniquet is not something that can be improvised. These actions need to be repeated, practiced, and fully integrated. Watching a video or taking an online course isn’t enough. The only way to truly understand the mechanics, the amount of pressure required, and the signs of success or failure is through hands-on training with the actual equipment.
Whether using a military-style tourniquet or a more versatile model, practical training and realistic simulation are essential to ensure safe, effective, and context-appropriate application in remote environments.
The tourniquet should be applied as early as possible—before signs of shock begin to appear. It must be placed directly on the skin, 5 to 6 cm above the wound, avoiding any joints. It should be tightened until bleeding stops completely, and the time of application must be recorded immediately.
All experts agree: it’s better to apply a well-placed tourniquet early than too late. Most importantly, the tourniquet is no longer seen as a last-resort measure, but rather as a temporary or definitive strategy for managing severe extremity bleeding—provided it’s used properly and followed by appropriate monitoring and, when possible, a context-appropriate plan for conversion..
What Types of Tourniquets Are There?
So-called “military” tourniquets, such as the Combat Application Tourniquet (CAT) or the Emergency Military Tourniquet (EMT) are the most
Military Tourniquet (EMT) are the most
reliables. They have been tested in high-stress situations and, when properly applied, can completely stop arterial blood flow.

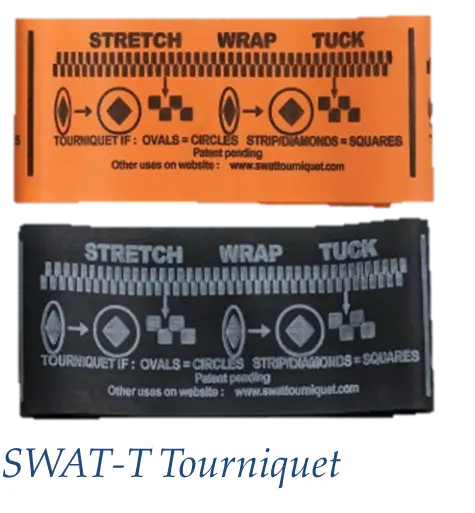
There are also more flexible models, such as the SWAT-T or the Slishman Pressure Wrap. These are often used by first responders or during expeditions. They are more compact and can function both as a tourniquet and as a pressure dressing. An insightful article by Adam Gent, from Real First Aid, shows that these models can be effective—especially when the user is well trained. Their application can be nearly as fast as military-style tourniquets (20 to 30 seconds), but their reliability tends to be slightly less consistent, particularly in the case of severe injuries.
In summary:
- For a hunting accident or a gunshot wound → a military-style tourniquet is recommended.
- For lightweight gear in remote settings → the SWAT-T or Slishman Pressure Wrap can be useful as complementary tools and offer more versatility.
In remote settings, it’s a different reality.
To fully understand what happens when a tourniquet is applied, two key points must be kept in mind:
- The tourniquet completely stops blood circulation beyond the point of application. Without oxygen supply, tissues begin to suffer quickly. This is known as ischemia, which can lead to cell death and irreversible damage if the tourniquet is left in place for too long.
- The tourniquet itself applies significant pressure to the skin, nerves, blood vessels, and muscles. This compression can lead to necrosis, nerve damage, deep muscle injury, or intense pain that is difficult to manage in the field.
In short, the tourniquet is a life-saving tool—but it comes at a cost. That’s why it’s essential not only to know when to apply it, but also when and how to remove it safely, If and as soon as the conditions allow. This process is known as conversion.
The real difference between an incident in an urban setting, a military context, and a remote environment is the time before evacuation to definitive medical care. In cities and many military operations, help often arrives quickly—so conversion isn’t usually a consideration. But in the forest, the mountains, or the tundra, the wait can last hours or even days.
When and How to Perform a Conversion
A tourniquet should never be removed arbitrarily. It should only be done if all of the following conditions are met:
- Stable – The person is stable (not in hemorrhagic shock).
- Control – The bleeding can be controlled with a well-applied pressure dressing or a hemostatic agent. In cases of amputation, do not attempt conversion.
- Monitoring – Someone is available to closely monitor the patient after the tourniquet is removed.
- Delay – Evacuation to definitive medical care will take more than 2 hours.
Although the two-hour mark is often cited as a safety threshold, complications can arise much sooner. And the six-hour window sometimes referenced in hospital settings does not apply in remote environments, far from surgical care.
Steps for a Safe Conversion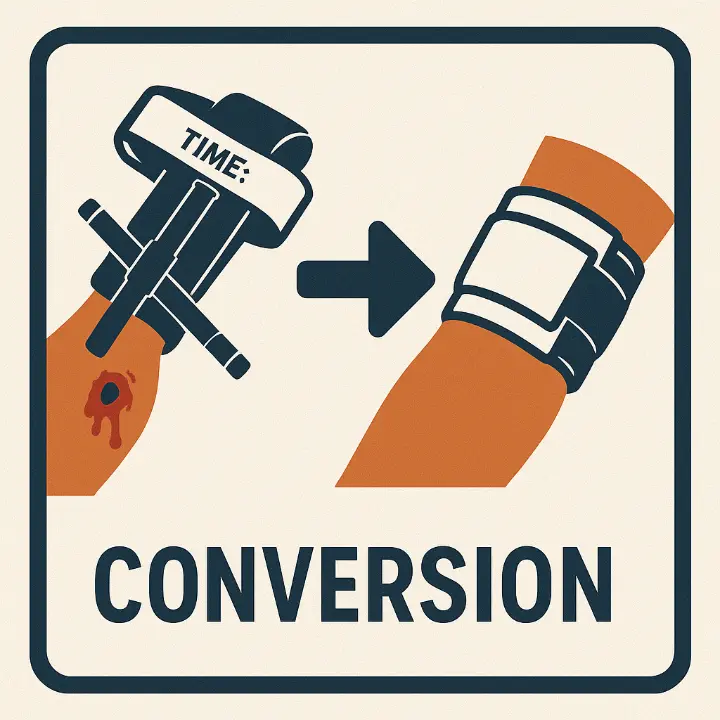
- Prepare a pressure dressing or a hemostatic agent.
- Apply it while the tourniquet is still in place, ensuring effective compression.
- Loosen the tourniquet slowly while observing closely.
- If the dressing becomes soaked with blood or visible bleeding resumes, immediately re-tighten the tourniquet.
- If the bleeding remains controlled, proceed with the conversion and apply manual pressure for 3 to 5 minutes if needed.
- Closely monitor the patient for 15 to 20 minutes, and continue continuous observation during transport or until definitive care is available.
- Reapply a tourniquet if bleeding resumes.
- Do not attempt another conversion if a properly executed initial attempt has failed.
- Remain vigilant afterwards
A successful conversion doesn’t mean the job is done. The minutes and hours that follow are critical to preventing complications. After removing the tourniquet, the patient must be closely monitored for skin colour, limb temperature, any recurrence of bleeding, or signs of severe pain or numbness. Any sudden change should prompt immediate action.
What You Should Carry in Your Kit
In high-risk settings (hunting, military, industrial, or technical/remote rescue operations), the tourniquet must be easily accessible—not buried deep inside a pack. Ideally, it should be carried on your person or secured to the outside of your kit, well protected but quickly reachable, because every second counts in the case of massive bleeding.

The contents of your kit should always be tailored to the activity: a hunting trip, an industrial deployment, a water-based rescue, an alpine expedition, or a remote backcountry hike all come with different requirements. Here are a few adaptable suggestions:
- Military-style tourniquet (CAT or EMT): Recommended for tactical situations, hunting, or any scenario with a high risk of serious injury.
- Versatile tourniquet (SWAT-T or Slishman): Useful as a lightweight or backup option for outdoor activities, expeditions, canoe trips, or climbing.
- Pressure dressings (ETD, OLAES, or improvised elastic bandages)
- Hemostatic agents (ChitoGauze, Celox): If the context and budget allow.
- Gloves, watch, pen, and a card to record the time of application
What matters most isn’t having everything—it’s having what you know how to use. One well-practised tourniquet is worth more than a bag full of gear you’ve never tested.
Decision-Making Under Pressure
Deciding whether to apply or remove a tourniquet is a serious responsibility. Even with experience, doubt is normal. That’s why hands-on training and simulation exercises are essential. The more you practise, the better you’ll be at making the right call—and the faster, safer, and more precise your actions will be.
What SIRIUSMEDx Recommends
At SIRIUSMEDx, we teach that:
- · The tourniquet is an essential life saving tool
- · It must be applied with sound judgment, not as a reflex.
- · Its conversion must be planned and carried out with care and precision.
Our training programs follow the guidelines of the TCCC and the Wilderness Medical Society, and are tailored to Canadian realities. We place strong emphasis on proper preparation, understanding the risks, and the ability to act methodically.
In remote settings, applying a tourniquet is the easy part. Knowing if, when and how to remove it safely requires skills that must be learned—and that’s exactly what we teach.

